Column: ‘No treatment until tragedy’ is our mental health system. CARE Court could change that

Fusako Petrus and a friend were taking their regular early-morning walk around a high school track here five years ago when a stranger came from behind and attacked them.
Petrus, 86, tried to fight off the assailant with a cane, but he turned on her, knocking her to the ground, stomping on her head and removing some of her clothing, in what authorities said was an attempted rape.
By the end of that day, Petrus was dead, and Sacramento County sheriff’s deputies had a suspect in custody: Neven Butler. Then 18, Butler was also charged in another assault that took place that afternoon, when he allegedly walked into an elderly care facility — where his grandmother and mom worked — and punched a 92-year-old woman in the face, then calmly returned to his mom’s car.
The random crimes Butler is accused of committing are painfully horrific, especially for the victims’ families and the community of North Highlands, where Butler and Petrus lived.
But behind that appalling day is another tragedy, one of our own making and responsibility. It goes to the heart of why Gov. Gavin Newsom’s proposal for a civil system of courts to handle cases of severe mental illness — CARE Court, short for Community Assistance, Recovery and Empowerment — isn’t just a good idea but a moral obligation.

Butler has been found incompetent to stand trial and is severely mentally ill, diagnosed with schizoaffective disorder, according to court and medical records I reviewed. Although Butler’s guilt or innocence is still undecided, in the days leading up to Petrus’ death, he had a questionable hold on reality.
If California had a reliable system of mental health treatment, and if Butler had been able to access it, he might not be facing a murder charge now. But there is no such system in this state. There is often no mandate that counties must actually provide treatment when someone like Butler needs it, and little accountability or liability for those that fail to do so. The services the government does provide are largely voluntary, with crater-size loopholes and convoluted caveats.
California’s current arrangement for handling severe mental illness is best described as “no treatment until tragedy.” It relies on sending our most severely mentally ill people into homelessness and police encounters — and eventual incarceration — as the most likely path to receiving help.
Thousands of families know this all too well, as do those in authority. Dozens if not hundreds of moms, dads, siblings, friends, officers, mental health advocates and others have told me of the maddening and absurd advice too often offered by law enforcement and even doctors: If a family wants help, have their loved one arrested.

If the CARE Court proposal, despite being flawed, can break that disgraceful and ugly pathway for even a few, it is irresponsible not to try it.
For nearly a year before the attacks, Butler’s mom, Brandi Michalik, tried to get him treatment. I met with her shortly after Butler was arrested and again recently, and her devastation was and is like a weight in the air around her. He is her only child, raised by her and her parents, Connie and Ray, in a house that was probably too small for all of them, but they made do.
Butler was a happy kid. You can see it in the photos that fill their shelves — a lineman on the football team who always brought friends home. He called his grandfather Poppa, and they were close.
A millionaire’s tax was helping fund new mental health programs in California. But the Great Recession changed things — and counties got desperate.
But Butler got into a car accident and later suffered a severe concussion at football. Maybe that had something to do with what happened next; maybe it would have happened anyway. At night, Brandi started hearing him talking and laughing to himself in the room next door. He began accusing her of things, strange things, like hiding a spaceship from him. He became afraid to leave his room and eventually, at times, refused to speak at all.
Brandi called his school for help, repeatedly. She took him to their doctor, who sent them to a counselor who saw him twice before Butler refused to go back. No one could make him, the counselor told Brandi. But Butler kept getting worse and Brandi more desperate.
Then one night, Butler came into her room and began punching her in the head until Ray pulled him off, Brandi said. She was left with the last resort that so many families dread: calling the police. Officers came and put Butler on a 5150 hold — basically, 72 hours in a locked mental health facility. From there, he was lucky enough to land a bed at an inpatient juvenile mental hospital.

Butler was put on one medication after another, but nothing seemed quite right. Three weeks later, he turned 18 and was released. Brandi had little say — her son was an adult and free to make his own decisions.
Butler came back to the bungalow. The next morning, and the day after that, Brandi said, she took him to the emergency room for side effects of the medication and continuing psychosis. She knew he wasn’t right, but she didn’t know what to do.
Nine days after being released, police say, Butler walked the 10 minutes from his house to his school and killed Petrus while Brandi was home taking a shower.
The discussion around CARE Court has focused on unsheltered people with severe mental illness and whether forcing them to accept treatment is ethical. But the proposal isn’t just about those on the street. It would allow families like Butler’s, who are unsuccessfully dealing with the mental illness of an adult, to petition the court for help before a person deteriorates to the point of homelessness or violence — those “upstream” of the streets and jails, as the advocates say.
More crucial, it requires counties to provide behavioral healthcare, housing and other services. That means a court order that mandates specific help for a specific person, potentially providing housing that includes an appropriate level of supervision. If the counties (or cities and other entities, depending on the service) fail to deliver on those orders, they can be sanctioned up to $1,000 a day and eventually have outside oversight appointed.
That accountability is something our system currently lacks, and that’s the part of CARE Court we should all be talking about. It’s what Sacramento Mayor Darrell Steinberg, the former leader of the state Senate and a decades-long mental health advocate, calls the “groundbreaking” part of the legislation.
“It’s madness to me that the current law enables everything to be bottom up and ‘Do the best you can,’” he told me. “Providing mental healthcare to people who need it the most is a voluntary act of government, and it shouldn’t be. It should be a legal requirement.”
After announcing the broad framework of his CARE Court plan, the real work begins for Gov. Gavin Newsom.
Steinberg said the state should create a legal right to treatment, giving people with severe mental health diagnoses the same standing as those with developmental disabilities. Currently, we provide services (also not enough, but legally obligated) such as regional centers and behavioral health treatment to those with developmental disabilities, acknowledging our responsibility to care for people unable to care for themselves.
CARE Court stops far short of a uniform right to treatment, but it does edge us closer. And from the cold, hard pragmatism of politics, it’s the best that can happen without a knock-down, drag-out fight at the Capitol over who exactly is gravely disabled when it comes to mental health — a battle the Legislature doesn’t want to have. So CARE Court is likely the best proposal we are going to get anytime soon.
Which brings us to forced treatment. The discussion around CARE Court has been focused on this point, with groups including the American Civil Liberties Union and Disability Rights California opposing the idea because they fear it infringes on the civil rights of those with mental illness.
It’s an important discussion. Taking away a person’s right to choose their own medical treatment, maybe even taking away their liberty in a locked ward, is an immense step.
But let’s go back to Butler. For five years, authorities shuttled him between the Sacramento County jail’s mental health floor and what is effectively solitary confinement, a type of isolated lockdown so egregious that the jail is under a consent decree to fix it.
Some prisoners go weeks without daylight or fresh air, according to a report on the decree, making their mental health so poor that some living in this “total separation” category are “smearing feces on the walls, hoarding food items and shrieking and banging on their cell doors,” guards and inmates say.
Butler is still not stable and is often mute — despite being ordered to take antipsychotic drugs, according to Brandi and court records. Though he was moved from total separation to another designation, Brandi calls it a change in name only, like “calling your pit bull ‘Fluffy Bunny.’”
In December, after years of arguing between the defense and prosecution, he was found incompetent to stand trial and ordered to a state mental hospital. He waited seven months for a bed and was finally transferred in early July.
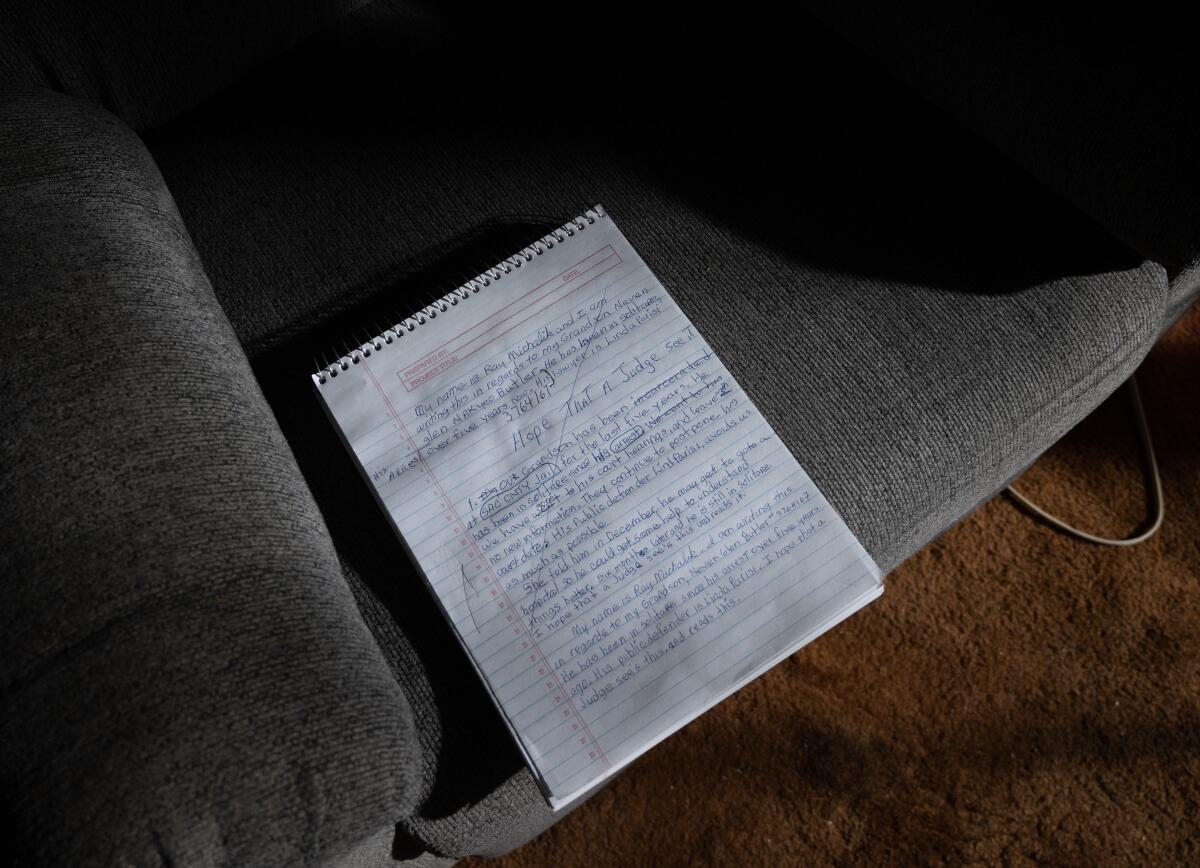
But Brandi has no idea where he is. The family heard he was at a facility in Napa, and Ray and Connie drove there, only to be turned away. Brandi was told that if she wanted to find her son, she should write a letter to every state hospital and wait to see if he responds.
“I am so disappointed with California and this broken, antiquated system,” Brandi told me Saturday, getting ready to mail those letters. She’s not giving up on finding him, but she feels like she’s “chasing a ghost.”
As of July 4, there were 1,739 people determined by courts to be incompetent to stand trial and waiting for space in a state hospital. Many have no idea how long they will be in limbo, and the treatment they get will be only enough to stabilize them so they can return to county jail and face trial.
So we have forced treatment in California, and a lot of it. It’s in our jails and prisons, and we disingenuously ignore it every day. Worse, we are using those jails to warehouse severely mentally ill people in a Kafkaesque state of uncertainty.
The Department of State Hospitals told me it currently houses about 4,499 patients who have been sent by courts for various reasons, plus about 900 determined to be incompetent to stand trial who are being treated in other locations. It has 4,434 beds in state hospitals for those patients and an additional 1,640 people participating in community-based treatment programs, some through jails and some outside lockdowns.
And those beds are nearly always full — so much so that the recent state budget allotted funds for 5,000 more spaces for diversion and community-based programs.
Gov. Gavin Newsom’s administration unveiled a plan to expand access to mental health care. It’s the opening play in an overdue discussion.
CARE Court gives people up to two years to work through voluntary treatment without criminalization. If after those 24 months, they are still not meaningfully taking part in their own care and stabilization, the court can send them to be considered for a conservatorship. That’s an entirely different court proceeding — through the Lanterman-Petris-Short Act — that allows both sides to present a case, represented by attorneys, before a decision is made.
If after two years a person is still so unstable that they can’t care for themselves, maybe we owe it to them to intervene.
The greatest challenge for CARE Court — and a real and urgent criticism — is that counties don’t have the resources to deliver on what a judge may require. We have a severe shortage of mental healthcare staff, including peer counselors, outreach workers and doctors, to handle the cases.
There’s clearly not enough housing, especially the kind with an array of services and supervision. And there is no stable funding stream. (Though Steinberg’s Proposition 63, the “millionaires tax,” is expected to bring in $3.8 billion this year for mental health funding, it’s a pot of money that fluctuates year to year.) County officials and especially behavioral care professionals worry that CARE Court will turn into a hot mess of legal orders made against a backdrop of scarcity — leaving them on the hook for problems outside their ability to fix or fund.
It will.
That’s the point.
Until someone forces the issue of inadequate funding and resources, California will continue to do what it has done for decades: Pass the buck.
So if it takes a judge ordering us to do better, I am all for it.
Because those people on the sidewalk — the naked ones, the raving ones, the ones covered in their own filth, the ones you are afraid to walk by because they seem genuinely threatening — a lot of them started out like Neven Butler. They came from families that loved them and love them still. They had troubles. No one helped.
And here we are.
This column is part of The Times’ mental health initiative, For Your Mind, an effort to increase coverage around treatment, public policy, wellness and culture related to mental health in California’s communities.
More to Read
Start your day right
Sign up for Essential California for news, features and recommendations from the L.A. Times and beyond in your inbox six days a week.
You may occasionally receive promotional content from the Los Angeles Times.